- Now let’s talk about pain -The doctors use the common 1-10 pain scale to tell them where your pain is at any given time. My PT’s talk about 3 parts of pain:
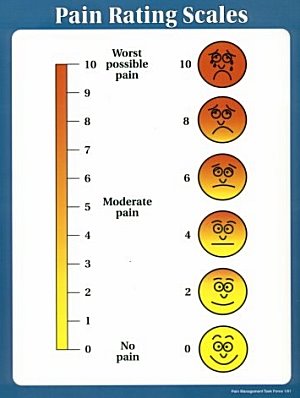
- 1) intensity of pain, is it a 1 or a 10 ----or somewhere in between
- 2) Frequency of flare-ups, Sometimes , all the time or am I in remission?
- 3) Duration of flare-ups. How long do they last? Keep a journal to recite all of these to your Dr or PT.
- The combination of these pain components will determine how the physician Rheumatologist, will treat the pain.
- The symptoms of RA pain can be treated with a myriad of medications to help control the pain. The most common types of these medications used for treating the symptoms of pain are non-steroidal anti-inflammatory drugs, (NSAIDS) and/or narcotic type of medications, Chemo- and others that accomplish some pain control are for long lasting control of the cells themselves.
- The other types of medications work directly on the diseased cells-http://en.wikipedia.org/wiki/Methotrexate Methotrexate is commonly used as the first round medication. Methotrexate is a low dose of chemotherapy that “slaps” the rheumatoid cells into submission and helps you feel better.Other Infusion medications & injectables are medications that are pumped into your system as maintenance drugs Humira, enbrel etc,. These are very effective and convenienr at keeping joint damage to a minimum & don’t have to be given as often as most RA medications. Some are in the form of pens that have single dose inside that you inject into your subcutaneous layer (fat) on your stomach, and some will require that you to go to an infusion facility where an I.V. of the RA medicine will be administered.. Your Rheumatologist will discuss medications with you in detail and you should investigate the side effects of the medicines – because there are quite a few.
- So, how can I control or limit the effects of RA with a minimum of drugs

- First of all RA treatment is a team effort between you, your family, your Rheumatologist, and your physical therapist. There is not a Not one size fits all approach to RA and you may have to keep trying combinations of treatment that work FOR YOU.
- One of the best ways to keep RA under control is to stay moving. When you hurt it seems like the last thing you want to do get up and get going. But you will find once you get out of your bed or chair and get moving around your joints won’t be as stiff, you have less RA symptoms and it will lessen the depression that sometimes accompanies RA, But fatigue and straess can make the RA flare up- So listen o your body and the choice is yours… lie around take lots of medications and feel miserable, or get up and moving and feel much better.
Get up and out early when you have Rheumatology and you wiull have a better dat
 |
- I find it very important to have a ritual to just to get out of bed and go get a coke or cup of coffee. It starts me off in a positive frame of mind and makes me feel better all day. This doesn’t mean I run around like a road runner-In fact, Fatigue and RA go hand in hand. But set a time limit to rest during those “down times” and you will find you’ll feel so much better

- · In the next blog- I have asked my Physical Therapist, Kale Isaacson to explain why movement of the Joint is so important for people with RA.
Footnotes: Autoimmune disease: http://en.wikipedia.org/wiki/Autoimmune_arthritis